(This chapter has 6 pages)
© Kenneth Todar, PhD

Borrelia burgdorferi, the spirochete that causes Lyme Disease. FA stain (CDC)
Introduction
Lyme disease was first recognized in the United States in 1975 by Dr. Allen Steere, following a mysterious outbreak of juvenile rheumatoid arthritis near the community of Lyme, Connecticut. The rural location of the Lyme outbreak and the onset of illness during summer and early fall suggested that the transmission of the disease was by an arthropod vector.
In 1982, the etiologic agent of Lyme disease was discovered by Willy Burgdorfer, who isolated spirochetes belonging to the genus Borrelia from the mid-guts of Ixodes ticks. He showed that these spirochetes reacted with immune serum from patients that had been diagnosed with Lyme disease. Subsequently, the etiologic agent was given the name Borrelia burgdorferi. Since then, reports of Lyme disease have increased dramatically to the point that the disease has become an important public health problem in some areas of the United States. Today, Lyme disease is the most prevalent tick-borne illness in the United States.

Incidence of Lyme Disease in the United States, 1991-2006. Lyme disease is the most prevalent tick-borne illness in the United States. In 2006, there were 19,931 new cases reported. Between 1996 and 2001 the average number was about 17,000 new cases per year but increased to near or above 20,000 new cases per year in 2002, probably due to increased surveillance and reporting. CDC.
Biology of Spirochetes
Borrelia burgdorferi, like the human pathogen Treponema pallidum, is a spirochete. Spirochetes are a group of phylogenetically-distinct bacteria that have a unique mode of motility by means of axial filaments (endoflagella). Spirochetes are widespread in viscous environments and they are found in the intestinal tracts of animals and the oral cavity of humans. The spirochetes have a unique cell surface which accompanies their unique type of motility. The endoflagella are contained within the periplasmic space between a semi rigid peptidoglycan helix and a multi-layer, flexible outer membrane sheath. When the filaments rotate within this space, the spirochetes move in cork-screw fashion. This type of movement is thought to be an adaptation to viscous environments, such as aquatic sediments, biofilms, mucosal tissues and the intestinal tracts of animals. For pathogens, this allows the spirochetes to hide their flagella, which are normally antigenic, from the host immune defenses.

Spirochetes are usually much longer than they are wide, and often their width is below the resolving power of the light microscope. For example, Borrelia may have a length of 20-30um but a width of only 0.2-0.3um. Hence, most spirochetes cannot be viewed using conventional light microscopy. Dark-field microscopy must be used to view spirochetes. Dark field microscopy utilizes a special condenser which directs light toward an object at a angle, rather than from the bottom. As a result, particles or cells are seen as light objects against a dark background.
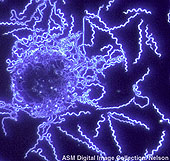
B. burgdorferi dark field illumination. American society for Microbiology.
The spirochetes are not classified as either Gram-positive or Gram-negative. When Borrelia burgdorferi is Gram-stained, the cells stain a weak Gram-negative by default, as safranin is the last dye used. Borrelia, like most spirochetes, does have an outer membrane that contains an LPS-like substance, an inner membrane, and a periplasmic space which contains a layer of peptidoglycan. Therefore, it has a Gram-negative bacterial type cell wall, despite its staining characteristics.
Cultivation
Unlike Treponema pallidum, Borrelia burgdorferi can be cultivated in vitro. However, the bacterium is fastidious and requires a very complex growth medium. The medium used to grow Borrelia burgdorferi is called Barbour-Stoenner-Kelly (BSK) medium. It contains over thirteen ingredients in a rabbit serum base. Borrelia burgdorferi has an optimal temperature for growth of 32oC, in a microaerobic environment. Even under optimal conditions, the generation time is slow, about 12-24 hours.
Borreliae from ticks and from the blood, skin, and cerebrospinal fluid of Lyme disease patients have been successfully cultivated in BSK medium. BSK solidified with 1.3% agarose allows the production of colonies from single organisms.
Strains of Borrelia
The borreliae causing Lyme disease are divided into several "genospecies", three of which have been firmly established and are well accepted:
I. Borrelia burgdorferi sensu stricto
II. Borrelia garinii
III. Borrelia afzelii
The term used to collectively describe all three genospecies is Borrelia burgdorferi sensu lato. The differences in genospecies are revealed by restriction fragment length polymorphism, (RFLP), multi-locus enzyme electrophoresis (MLEE) and ssRNA sequences. All U.S. isolates fall into genospecies I. Examples of all three genospecies have been found in Europe and Asia, although II and III predominate there.
Outer Surface Proteins
The outer membrane of Borrelia burgdorferi is composed of various unique outer surface proteins (Osp) that have been characterized (Osp A through OspF). They are presumed to play a role in virulence. Osp A and Osp B are by far the most abundant outer surface proteins. The genes encoding these proteins are transcribed from a common promoter and are located on a 49 kb linear plasmid. The chromosome of Borrelia burgdorferi is also linear and is almost 1100 kb in size.
Pathogenicity
Borrelia burgdorferi invades the blood and tissues of various infected mammals and birds. The natural reservoir for Borrelia burgdorferi is thought to be the white-footed mouse. Ticks transfer the spirochetes to the white-tailed deer, humans, and other warm-blooded animals after a blood meal on an infected animal. In humans, dogs, and many other animals, infection with Borrelia burgdorferi results in the pathology of Lyme disease.
Incidence and Distribution of Lyme Disease in the United States
Lyme disease has a wide distribution in northern temperate regions of the world. In the United States, the highest incidence occurs in the Northeast, from Massachusetts to Maryland and the North-central states, especially Wisconsin and Minnesota.
In 2002, more than 23,000 cases of Lyme disease were reported in the U.S., the highest number ever reported. This increase could be caused by an increase in human contact with infected ticks and enhanced reporting of cases.
Ten states have consistently reported an incidence of Lyme disease higher than the national average: Connecticut, Delaware, Maryland, Massachusetts, Minnesota, New Jersey, New York, Pennsylvania, Rhode Island and Wisconsin. During 2003-2005, 64,382 Lyme disease cases were reported to CDC, of which 59,770 cases (93%) were reported from these 10 states. Similar data was reported in 2006 (see map below).

Lyme disease cases by state, 2006. CDC.http://textbookofbacteriology.net/Lyme.html
No comments:
Post a Comment